This is a story about overcoming fear, beating the odds, and finding inner strength.
As I lay on the hospital bed, a lavender-scented pillow resting over my eyes, legs raised in the air, I realized that infertility was my battle. Infertility was my fight.
I was a marketing director living a picturesque life in Bend, Oregon. I gardened in the summer and cross-country skied in winter. I ate organic everything and practiced yoga daily. I was infertile.
Month after month, I'd hope for two intersecting lines on the pregnancy test only to be crushed. Again and again.
Pregnancy announcements poured in at the same rate as my tears. Everyone was pregnant, but me. I wanted to be happy for my friends, but I was so sad for myself and couldn’t ignore those emotions. I felt myself retreating; I needed answers.
I contacted one of two doctors in Bend who specialized in infertility and booked the next available appointment, which was two months out. In the meantime, I met with the family planning nurse who suggested acupuncture. Maybe that's all I needed, she assured me.
At acupuncture, I met Sharyn Allyson who became one of the greatest supporters of my struggle. Sharyn kept me calm, she laughed with me and cried with me; she listened to my hopes, dreams, and fears. Sharon was a huge proponent of Chinese medicine and natural healing, but she helped open my mind to medicated treatments. Little did I know the complicated road that lay ahead.
Two months had gone by and it was finally time to meet with the fertility doctor in Bend. He reviewed my blood work and ultrasound. Finally, some answers. Polycystic ovarian syndrome (PCOS) was the likely cause of my infertility. I wasn't a textbook case, but anovulation (missed periods) and string-of-pearl cysts on my ovaries were two signs. My follicles were tiny and didn't seem to mature, and my cycles were long, sometimes 40+ days.
I never thought I'd go through with Clomid and IUIs, let alone IVF, but there I was with my back against the wall, deciding to give Clomid a try. The Clomid Challenge Test seemed promising - I'd take a low dose of Clomid to make my ovaries produce stronger, bigger follicles. My doctor suggested that maybe that was all I'd need to get pregnant. I was hopeful, but I didn't get pregnant.
Two rounds of Clomid later and still not pregnant, I prepared for my first IUI (intrauterine insemination). In this procedure, the doctor used a catheter to place the sperm next to the eggs in my uterus. He doubled my dose of Clomid and I injected myself with a "trigger" shot 36 hours before the procedure to jump start ovulation. I still didn't get pregnant.
Every month, I'd be so hopeful. We tried another IUI on my next cycle, only to be crushed by another single line on the pregnancy test.
Femara, that was the next drug we'd try. It was similar to Clomid but could produce better results, the doctor explained. We started off with a hefty dosage, and then came the follicle checks. Although we'd planned to do a third IUI, my follicles didn't react to the Femara so we canceled the procedure. We waited for my next cycle and upped the dosage of Femara to the maximum. Unfortunately, my body barely registered the drug again, and we canceled another IUI.
It had been nine months of failed fertility treatments. And right on queue, newborn baby announcements started rolling in. My closest friends were celebrating their highest highs while I was at my lowest low.
I was at the bottom of a dark place. I tried to imagine life without my own child. I'd helped raise my stepdaughter since she was 14. I loved her beyond words, but for the past three years, my biological clock was an alarm waking me each morning, impossible to ignore.
I never knew how badly I wanted a baby until I couldn't have one.
My doctor suggested IVF (in vitro fertilization) given our failed attempts at IUI. He explained that while we could continue with IUIs, our lack of success up to that point meant the odds were only getting worse. IVF had much higher success rates.
The closest IVF clinic was three hours away in Portland, and then there were the financials. We'd already spent a few thousand on fertility treatments in Bend and IVF would set us back $15,000 more. Add to that transportation and overnight stays, which would total close to three weeks. That's not to mention the counseling I might need down the road. Up to 50% of IVF patients experience symptoms similar to PTSD, and an infertile diagnosis can affect women the same way a cancer diagnosis can. I wondered if I could handle all of this logistically, financially, and most of all, emotionally.
We set up an introductory Skype call with Dr. Bankowski at Oregon Reproductive Medicine (ORM). By then, my friends were uploading photos of their babies to photo sharing sites while my fate was still in limbo. Would IVF work? Would I be one of the lucky ones?
Dr. Bankowski gave us a run down of the IVF protocol that would take place over the next six months. If all went as planned, we'd have a 68% chance of success. This was far better than the 10% success rate of IUIs and I felt hopeful once again.
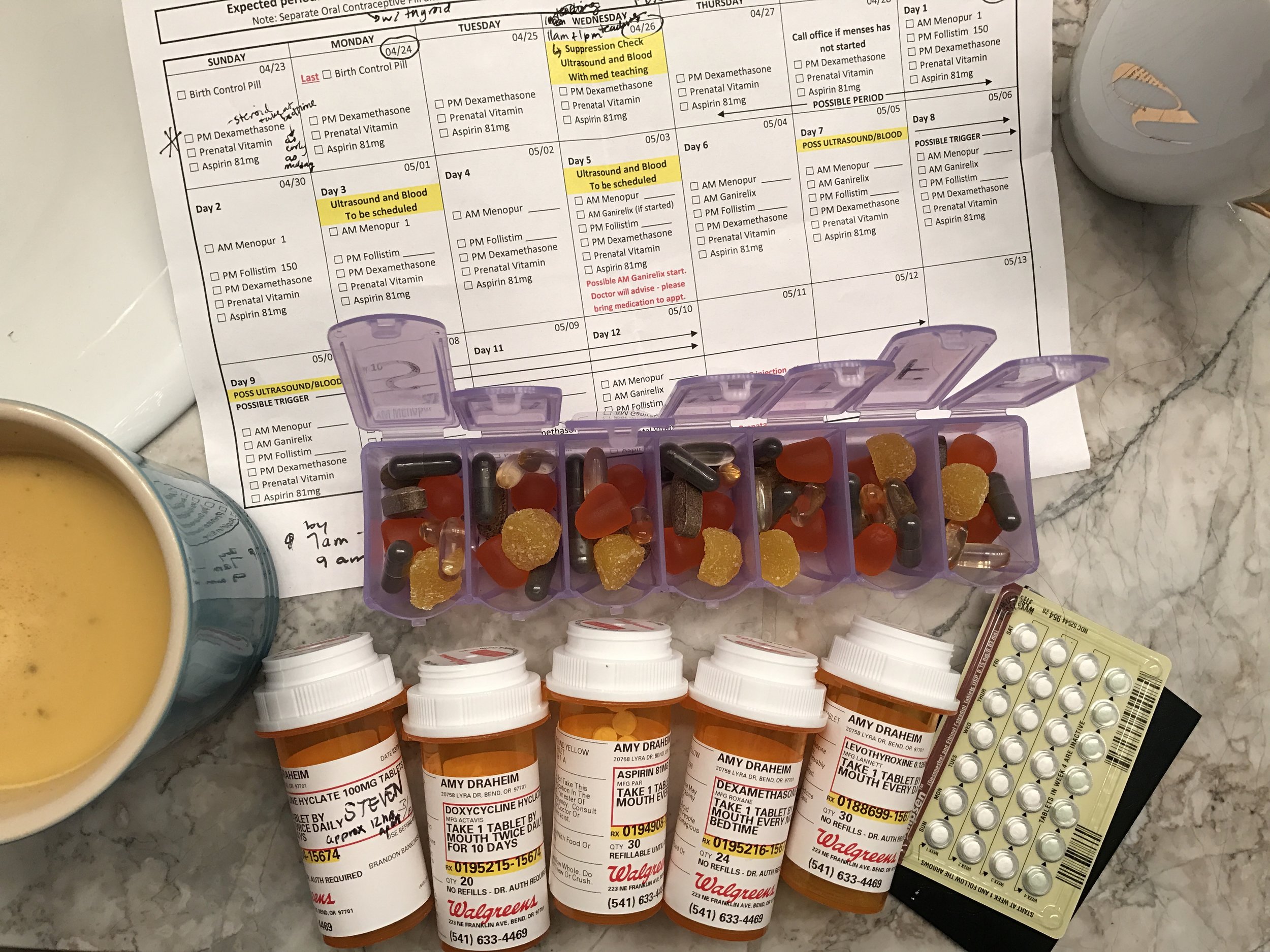
Along with a much higher success rate, the IVF process would be much more intensive and intrusive. There were several steps that surprised me, including going on birth control for a month to suppress my follicle production before stimulating it, putting my husband and me on an antibiotic to prevent against infection, putting me on a steroid, and only then preparing for egg stimulation and extraction.
The stimulation involved injections I'd need to administer, up to four per day, into my abdomen. They included Menopur, Gonal F, and Ganirelix. Combined, they'd plump up my follicles and increase my egg count. My ovaries would go from the size of walnuts to the size and consistency of water balloons. I was warned against strenuous exercise lest my ovaries get twisted or snap. Ouch!
In the two weeks leading up to the egg extraction, I was monitored every other day with a blood draw and an ultrasound to check the quantity and quality of my follicles. Within the first few days, around a dozen follicles were visible and growing in each ovary. Finally, progress.
My mornings and evenings revolved around injections. It was an elaborate process. First, I'd numb the area, then I'd bring the meds up to room temp, draw the correct dosage, inject, release, and then apply a hot compress to reduce the pain and bruising. I'd do it all again that evening.
With all of the monitoring, I ended up renting an Airbnb in Portland for two weeks. A six hour commute to and from Bend/Portland every other day just didn't make sense.
My sister flew in to spend a week with me before my husband arrived for the surgery. Despite the daily injections, my sister kept my spirits high. We went on walks and explored Portland's hipster scene. We cooked at home and watched episodes of our favorite shows. Miraculously, Portland's rain clouds parted and we enjoyed some sunshine. We even went on a couple of day trips.
The Wooden Shoe Tulip Festival was one place I'd always wanted to visit and I knew that being there would brighten my outlook. Tulips spread out like a colorful sea, and for a moment, we were just two sisters on a road trip together.
We also ventured out to the Oregon Coast and had a picnic on Cannon Beach. We did a little tide pooling, had a photo shoot, and snacked on steamed clams before heading back to Portland.
Looking back, my sister was a major factor in the positive way I received and responded to the medicine and the appointments. I hope someday I'll be able to return the favor.
Two weeks had gone by, and it was almost surgery day. My follicles had reached the size the doctors were looking for, and I was once again injecting my trigger shot (at exactly 10:15 p.m. the night before), to kick start ovulation.
Steven and I arrived on the second floor of ORM the next morning and were whisked away to our room. I had been given very clear instructions not to have any scented products on my skin - no nail polish, no makeup, and no contact lenses - to keep the operating room as sterile as possible. The slightest imbalance could decrease the viability of the eggs, so it was important not to introduce any fragrances or chemicals into the room.
Cherry blossoms bloomed outside of our window. The nurse explained the surgery and the post-operation protocol as she inserted an IV into my hand. I'd be wheeled into the surgery room, put under with general anesthesia, and the doctor would perform the extraction. He'd enter my ovaries, poke a needle into each follicle, and suck out the eggs with a tiny vacuum. He'd proceed to do this into every follicle, and before we left the clinic, we'd know how many eggs had been successfully extracted.
I looked at Steven as tears welled up in my eyes. This was really happening. I couldn't remember a time in my life that I'd been given general anesthesia. I was hopeful for the outcome but, after so many failures in the past year, nervous that my body might fail me again. I was thinking about the future too - about our future child and how I'd share this story with him or her someday.
Before we knew it, the doctor had arrived wheeled me away. I remember classical music and bright lights. The nurses lifted my legs into stirrups and my eyelids got so heavy that I finally gave in. The light faded to black.
The next thing I knew, Steven was standing over me. We were back in the waiting room. He smiled and told me were were finished. I was still pretty heavily drugged. How many eggs had they retrieved? In my haze, I must've asked three times.
37 eggs were successfully extracted. Out of those eggs, 31 were mature. Steven had done his part in another room during the surgery. The sperm met the egg in the laboratory minutes after the extraction, and 24 out of the 31 mature eggs were successfully fertilized.
From there, the 24 fertilized eggs would stay in the lab for the next five days. Over that time, approximately 40-50% would prove themselves viable by staying alive, and the five day old embryos would be sent to a lab for genetic testing which would take up to two weeks. Talk about a journey. After that, we'd know how many "good" embryos we had, and they'd be scored by their individual viability - A, B, C and so on.
My Portland chapter was over for now, and it was time to head back to Bend and wait for the results. I was given ibuprofen and Tylenol with codeine for the pain, and was told to stay in bed for the next couple of days. There was a risk of ovarian hyperstimulation syndrome (OHSS) from the follicles that had been harvested, so bedrest was a non-negotiable. Over the next five days, the pain got worse before it got better, but eventually it subsided.
Then I got the call. Out of 24 fertilized eggs, 13 made it to day five and were being sent for genetic testing. Finally, I had more positive news. I celebrated with a rare glass of wine that night (I hadn't drank for over a year, wishfully thinking I might be pregnant each month), and texted my friends and family. I felt a sense of relief that I hadn't felt in months; IVF was working after everything else had failed.
About 10 days later, I received a call from ORM. Out of 13 embryos, two were abnormal and would be discarded, two were mosaic (the success of which was still a bit fuzzy scientifically speaking), and nine were normal.
The nine normal embryos would be the pool from which we'd implant into my body.
"Would you like to know the genders?" The nurse asked over the phone.
"Yes," I said, my heart racing.
"You have four boys and five girls," she said without skipping a beat.
I felt my chest get hot. Tears began pooling in my eyes, "Okay, thank you," I said, my voice shaky, "Did you score them yet?"
"Oh, yes," The nurse said, "They're all AA, which is the highest quality they can be," she added.
The call ended. And I cried. And cried and cried. I called Steven and through my tears shared the good news.
We needed to decide how many embryos to implant and which gender(s). IVF had come a long way in recent years. The odds of one embryo's success was 68% with a 2% chance of twins. Implanting two embryos would increase the chance of success to 82%, but the risk of twins would increase to 60%. Steven and I agreed on one male embryo and completed the associated paperwork (including getting it notarized - this was serious stuff). Down the road, if we wanted another baby, we'd have eight more embryos waiting for us at ORM.
The next day, our nurse called with the details of the IVF transfer. Over the next month and a half, ORM prescribed a series of injections, namely estrogen and progesterone. This time, I'd administered them intramuscularly into my upper butt (that may not be the scientific term). These injections would trick my body into thinking I was pregnant. Then came the embryo transfer.
If all went as planned, my body would accept instead of reject the embryo and two weeks from the transfer date, a blood test would confirm that I was successfully pregnant for the first time in my life. The transfer date was set for July 6, 2017.
The days leading up to the transfer were important. I wanted to have some stress-free time with my husband. July 2nd marked my 34th birthday, and with the transfer just a few days later, we decided to make a vacation out of it. We headed to the Oregon Coast for a couple of nights at Salishan Resort.
Since relaxation was the doctor's orders, we scheduled massages at the spa and took long walks on the beach. We savored dinners with ocean views, played tennis, and otherwise took it easy.
After a few days of R&R, we headed to Portland. The evening before the procedure, we went out for happy hour and then to dinner at Andina, a Peruvian restaurant in Portland's Pearl District.
We'd purchased tickets to a professional soccer game later that evening. Attending a game in Barcelona was one of our favorite memories of all time, and since I'm nostalgic to a fault, walking into the stands took me right back. Back to Spain, and back to a time when I wasn't injecting myself or worrying about getting pregnant.
The game relieved us both of the weight of what was happening the next day. In the Timbers souvenir shop, we couldn't resist a pair of tiny slippers for our son. Maybe someday we'd take him to a game in Portland or even Barcelona.
We didn't need to arrive at ORM until the afternoon the next day, so we got up early and went for a hike on Mt. Tabor. Walking the paths, I took some deep breaths and centered myself. It was one of the most important days of my life. In a few hours, I'd finally be pregnant after over four years of trying. My dream of becoming a mother to my own baby would finally come true.
We arrived at ORM and were brought to our room. I'd opted to have acupuncture immediately before the transfer and again immediately after. I'd read some research that IVF transfers could be up to 200 times more successful with pre and post acupuncture treatments. I'd take those odds. Dr. Bankowski arrived and I was ready for the transfer.
For this procedure, I wouldn't need anesthesia, in fact the transfer would only take a few minutes and then I'd need to rest. Steven had changed into the provided scrubs and stayed by my side as the nurse wheeled me into the operating room. Steven took a seat by my head and held my hand tightly.
Dr. Bankowski addressed us with a smile. "There's your embryo," he gestured. We looked up to see our embryo projected onto the wall. Steven squeezed my hand and we shared an emotional sigh. Tears welled up in both of our eyes.
The transfer was done and I was wheeled back to the waiting room. The acupuncturist returned and needled me again. About 45 minutes had passed when the nurse arrived to help me to the bathroom. When I was finished, a wheelchair was waiting.
We were ready to go. The nurse wheeled me across the street to Hotel DeLuxe where I stayed on bedrest for the next 48 hours.
Steven made sure I was comfortable, ordered takeout, and headed out to pick it up. He returned and the delicious smells of mediterranean food filled the room. He held the takeout in one hand and in the other, a bouquet of flowers and a gift box. The flowers were beautiful and the gift was a tiny, knit onesie with a whale on the belly. I imagined what it would be like for our baby to wear this little outfit someday. We noshed on Israeli food and shared more emotional tears.
Steven left for Bend that evening and some of my best friends arrived shortly after to keep me company.
The next two days went something like this: room service, movies, laughter, progesterone injections, more laughter, more room service, more movies, more take out, all while remaining horizontal.
Two days passed with the blink of an eye. We headed out for brunch before hitting the road. It had been an incredibly emotional and meaningful week, and I was ready to go home.
Back in Bend, I waited anxiously for my two week appointment. When the day came, I reported to the local hospital for blood work. My HCG and beta levels would indicate that I was still pregnant. All of the tests were positive. My beta levels were tripling every two days. I continued the progesterone and estrogen shots until the end of the first trimester, but the levels were tapering down. The injections had become second nature.
About a month after the transfer, we were back at ORM in Portland. I was six and a half weeks along, and the ultrasound revealed a healthy baby. The sound of his tiny heart beat echoed in the room.
"Congratulations," Dr. Bankowski told us, "He has a very strong heart beat."
I was pregnant. After four years of trying, I was finally pregnant. A part of me never thought I'd get to write those words.
I never knew how badly I wanted a baby until I couldn't have one. I had no idea that this would be my path. And now, as I type this, and as my baby boy sleeps soundly by my side, I have to pinch myself. I have to take some deep breaths, remind myself to honor my journey, and never lose sight of the path that brought us to this precious moment.
And now, to show our baby the world...
Like this post? Pin it.